Hearing Testing
Timothy C. Hain, MD
Last edited: 9/2008
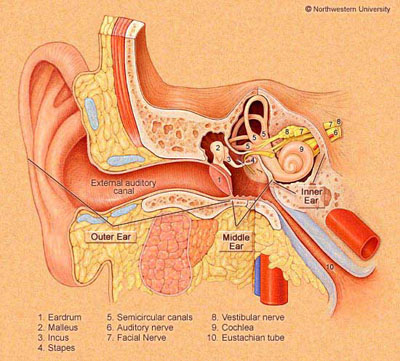 |
| Figure 1. The Ear. Hearing can be impaired due to lesions in the external ear canal, the middle ear, or the inner ear. The purpose of hearing testing is to evaluate hearing function and, if it is impaired, to attempt to localize the site of lesion.
|
What is Hearing Testing?
Hearing testing is a means of evaluating an individual's overall hearing function. The tests are used to determine if there is something wrong with the hearing (auditory) portion of the inner ear. They are often used as an initial screening to decide if more expensive tests like magnetic resonance imaging (MRI) are needed. They are sometimes used in conjunction with vestibular testing to diagnose specific disorders, such as Meniere's disease. Finally, hearing tests can be used to decide if a hearing aid might be helpful.
The following hearing tests are briefly described below:
- Bedside testing
- Audiometry
- Tympanometry
- Brainstem auditory evoked response (BAER)
- Electrocochleography (ECOG)
- Otoacoustic emissions
Bedside Testing of Hearing
There are many ways of testing hearing in the office. Bedside testing may be used as a screening procedure. While formal audiometry is preferable, for reasons of expense or access, it may not always be possible. In bedside testing, tuning forks (Figure 2) are often used to test at chosen frequencies. A variety of other methods (whisper, rubbed fingers, ticking watch, and so forth) can be used to quantify hearing using readily accessible sources of noise.
 |
Figure 2:
Three different sized tuning forks. The higher pitched forks (such as the 512 hz fork) are more appropriate for hearing testing. (c) Timothy C. Hain, MD. 2002 |
The single most common office test is a tuning fork test called the Rinne, named after Adolf Rinne of Gottingen, who described this test in 1855. In the Rinne test, a comparison is made between hearing elicited by placing the base of a tuning fork applied to the mastoid area (bone), and then after the sound is no longer appreciated, the vibrating top is placed one inch from the external ear canal (air). A positive Rinne test indicates an air-bone gap and, therefore, presumed presence of a conductive hearing loss. Frequencies from 256 to 1024 Hz have been advocated as appropriate for testing. When the air-bone gapis less than 17.5 dB or greater than 30 dB, the Rinne is usually negative (Jacob et al, 1993). Because of this, the Rinne test has limited utility.
In the Weber test, a 512 Hz tuning fork is placed on the patient's forehead. If the sound lateralizes (is louder on one side than the other), the patient may have either an ipsilateral conductive hearing loss or a contralateral sensorineural hearing loss.
Other tuning fork tests include the Bing and Schwabach tests. In the Bing test, the fork is struck and placed on the patient's mastoid tip. The examiner alternately occludes the patient's external meatus. If the patient has normal hearing or a sensorineural loss, he or she will notice a change in intensity with occlusion. If the patient has a conductive hearing loss, he or she will notice no change.
The Schwabach test compares the patient's bone conduction to that of the examiner's. If the patient stops hearing before the examiner, this suggests a sensorineural loss. If the patient hears it longer than the examiner, this suggests a conductive loss. Of course, this test is contingent on the examiner having normal hearing.
Recent studies have evaluated the effectiveness of specific bedside tests. Screening tests that proved useful include the whisper test (Bagai, 2006; Pirozzo, 2003), audioscope/audiometer and self report questionnaires (Yueh, 2003). These are good tests to use initially in the evaluation of hearing loss.

Audiometry
Figure 3:
Audiogram for a Patient With Normal Hearing
COMMENTS: DNT
= did not test. Pounding heartbeat right ear - constant. No evidence of heartbeat rhythm in tympanogram.
|
Audiometry is the term used to describe formal measurement of hearing. The measurement is usually performed using an "audiometer" by an "audiologist". In audiometry, hearing is measured at frequencies varying from low pitches (250 Hz) to high pitches (8000 Hz). An example of an audiogram in a person with normal hearing is shown in figure 3. The hearing level is quantified relative to "normal" hearing in decibels (DB), with higher numbers of DB indicating worse hearing. The DB score is not really percent loss, but nevertheless 100 dB hearing loss is nearly equivalent to complete deafness for that particular frequency. A score of 0 is normal. It is possible to have scores less than 0, which indicate better than average hearing.
Figure 4:Audiogram for a Patient With an Acoustic Neuroma
|
Figure 4 illustrates an audiogram of a person with a tumor called an acoustic neuroma. Hearing is worse for the left ear (squares) than the right ear (circles) although both ears are at least partially outside the normal range.
When there is a hearing loss, the next step is to try and determine whether the loss is caused by a sensory problem (sensorineural hearing loss) or a mechanical problem (conductive hearing loss). This distinction is made by using a bone vibrator, which bypasses the mechanical parts of the middle ear. If hearing is better using bone than air, this suggests a conductive hearing loss.
Routine audiometry, like routine eye care, is often not covered by health insurance in the United States. When audiometry is performed for specific medical reasons (for example, to follow Meniere's disease), it may be covered.
There are a number of special subtests that are optionally included in the audiometry procedure. Speech audiometry involves reading a list of words to see if patients can discriminate words. By comparing speech comprehension with anticipated speech comprehension, inferences can be made about central processing and central hearing deficits.
Acoustic reflex testing consists of subjecting the ear to a loud sound and determining if it causes the stapedius muscle to tighten the stapes. Acoustic reflexes are mainly useful as a crude but non-subjective method of evaluating hearing, as the stapes should tighten for a given level of perceived loudness. Acoustic reflexes can also be a sign of brainstem dysfunction. Click here for more detail.

Tympanometry
 |
Figure 5:
Tympanometry from case of figure 4 above.
|
Tympanometry is a measure of the stiffness of the eardrum and thus evaluate middle ear function. This test can be helpful in detecting fluid in the middle ear, negative middle ear pressure, disruption of the ossicles, tympanic membrane perforation, and otosclerosis.
To perform the test, a soft probe is placed into the ear canal and a small amount of pressure is applied. The instrument then measures movement of the tympanic membrane (eardrum) in responses to the pressure chances.
The result of the test is recorded in a visual output, called a tympanogram. If there is fluid in the middle ear, the tympanic membrane will not vibrate properly and the line on the tympanogram will be flat. If there is air in the middle ear (the normal condition) but the air is at a higher or lower pressure than the surrounding atmosphere, the line on the tympanogram will be shifted in position.
 |
Figure 6:
Brainstem auditory evoked response.
Right ear responses are shown on top and left ear on the bottom half.
|
Brainstem Auditory Evoked Responses (BAER or ABR)
Brainstem auditory evoked responses (BAER),also known as auditory brainstem evoked response (ABR), measures the timing of electrical waves from the brainstem in response to clicks in the ear. Three waves (1, 3 and 5) are plotted for each ear. Delays of one side relative to the other suggests a lesion in the 8th cranial nerve between the ear and brainstem or the brainstem itself. The main indication for BAER is when an acoustic neuroma is suspected. However, MRI is a superior test for this purpose. BAER testing may also be useful in situations where an auditory neuropathy is suspected. In this case, it may be combined with otoacoustic emission testing (see below). BAER testing requires reasonable high-frequency hearing.
An example of an abnormal BAER (for the left ear ) is shown in Figure 6.
Electrocochleography (ECOG)
ECOG is a variant of BAER where an electrode is placed on or in the ear drum to increase the size of wave 1 of the BAER. ECOG can be used to diagnose Meniere's disease and related conditions. ECOG is a difficult technical procedure and for this reason is not always helpful. ECOG is also only useful diagnostically when positive.
Otoacoustic Emissions
This is a relatively new test used to assess hearing in newborns as well as being a method of determining whether the cochlea is functioning. With this test, a probe that contains both a tiny speaker and a tiny microphone is inserted into the ear canal. Quiet tones are sent from the speaker, which travel through the middle ear and stimulate the hairs in the cochlea The hairs respond by generating their own minute sounds, which are detected by the microphone. If there is a hearing loss, the hairs in the cochlea do not generate these minute sounds. Otoacoustic emissions testing can be used to monitor hearing response to treatment and can aid in choosing the appropriate therapy (Kemp, 2002).
Acknowledgments
Figures 1,3 and 4 are courtesy of Northwestern University, and were assembled by Pam Fiebig, Senior lecturer in Audiology. The remainder of the figures are copyrighted to Timothy C. Hain, MD
References
- Bagai A, Thavendiranathan P, Detsky AS. Does this patient have hearing impairment? JAMA. 295(4):416-28, 2006.
- Jacob V, and others. Can Rinne's test quantify hearing loss? ENT journal,
1993, 152-153
- Kemp DT. Otoacoustic emissions, their origin in cochlear function and use. Br Med Bull. 63:223-41, 2002.
- Pirozzo S, Papinczak T, Glasziou P. Whispered voice test for screening hearing impairment in adults and children: systematic review. BMJ. 327(7421):967, 2003.
- Yueh BM, Shapiro N et al. Screening and management of adult hearing loss in primary care:scientific review. JAMA. 289(15):1976-85, 2003.

|